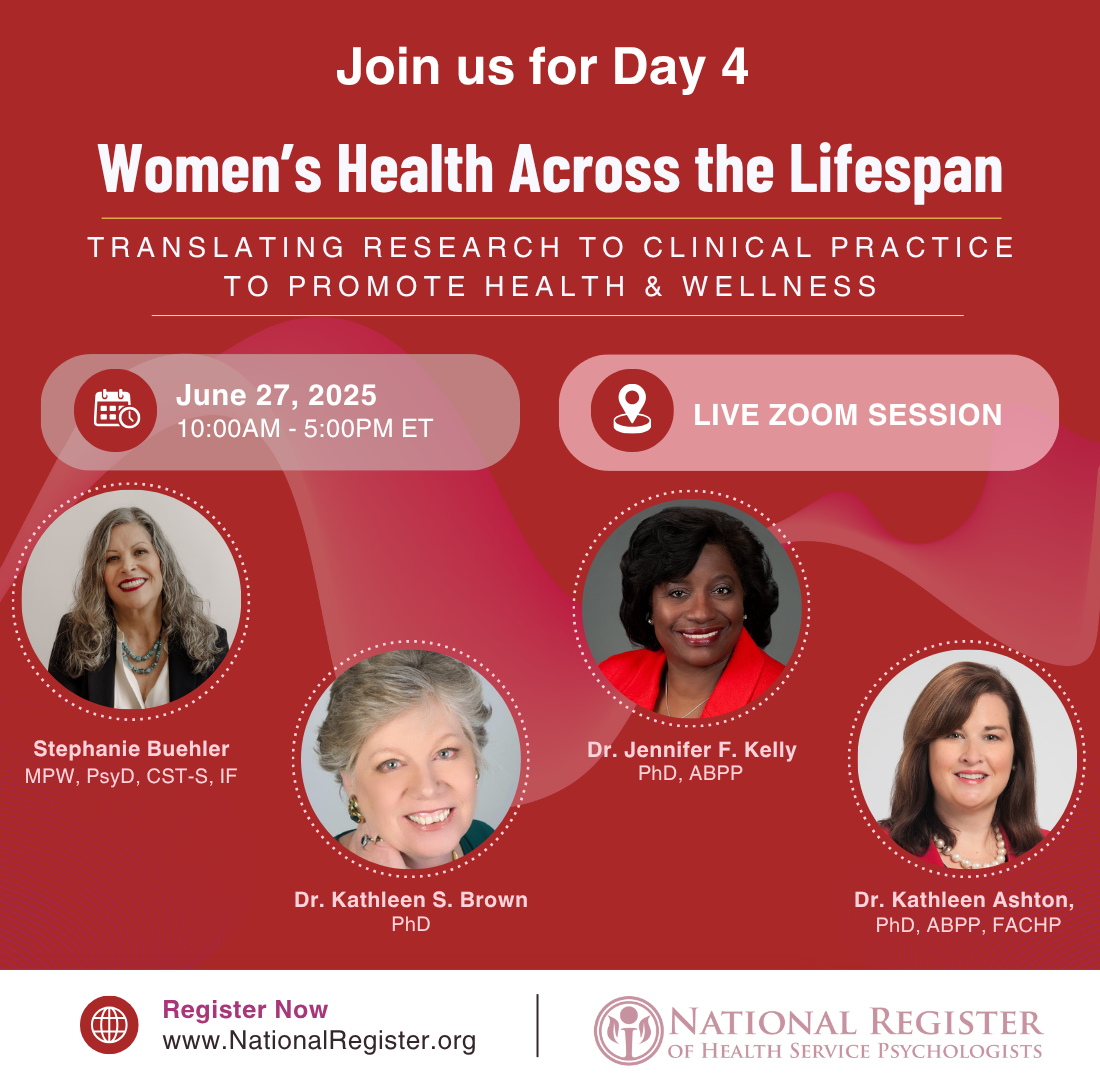
The National Register is excited to announce Women’s Health Across the Lifespan: Translating Research to Clinical Practice to Promote Health and Wellness, a multi-day educational event focused on translating evidence-based research into clinical practice to promote and address women’s health across the lifespan. This program, developed in collaboration with Helen L. Coons, PhD, offers participants the opportunity to earn up to 22 CEs across five daylong sessions held over five months.
Each day focuses on a specific area of women’s health, offering insights and practical tools for psychologists. This unique opportunity to advance your expertise in women’s health features dynamic speakers with expertise in sex and gender aspects of women’s health who will translate cutting-edge research and guidelines on biomedical, psychosocial, behavioral, and sociocultural aspects of women’s health and wellness for your practice. Case examples will highlight clinical strategies to promote wellness in women from a variety of communities and identities. Presenters will also discuss best practices for communicating with interprofessional women’s health care providers and settings.
Register for all five days at a discounted price ($650 member/$775 nonmember) or register for select days at a per-day price ($150 member/$175 nonmember). Registration is for live events only, which will occur 10am-5pm EASTERN Time.
Review all session details below or jump to a specific day: March 28 | April 25 | May 30 | June 27 | July 25
Dr. Teni Davoudian will focus on the assessment and evidence-based psychological treatment of perinatal mood and anxiety disorders (PMADs). Associated risks and mitigating factors of PMADs will be reviewed. Case studies of women with PMADs will be presented for discussion.
2 CE Credits, Instructional Level: Intermediate
2 Contact Hours (New York Board of Psychology)
Learning Objectives:
Disclosures: Dr. Davoudian has no conflicts of interest to disclose.

Teni Davoudian, PhD, ABPP, is a board-certified health psychologist specializing in reproductive mental health. In 2014, Dr. Davoudian obtained her PhD in Clinical Psychology from Marquette University. Currently, Dr. Davoudian is an Associate Professor in the Departments of Obstetrics & Gynecology and Psychiatry at Baylor College of Medicine and serves as the Director of Psychological Services within Baylor’s Division of Reproductive Psychiatry. She provides psychotherapy and assessments to perinatal, fertility, uterine transplant, and perimenopausal patients.
Dr. Melissa Kwitowski will focus on the interplay between acute and chronic physical health conditions among birthing persons in the setting of fertility and family planning and will focus on the unique facets of obstetric care and delivery for these patients. She will also highlight clinical considerations when working with this population. Dr. Kwitowski will discuss topics related to medical trauma, patient autonomy and advocacy, and interactions with the medical system.
1 CE Credit, Instructional Level: Intermediate
1 Contact Hour (New York Board of Psychology)
Learning Objectives:
Disclosures: Dr. Kwitowski has no conflicts of interest to disclose.

Melissa Kwitowski, PhD, is a licensed psychologist and Assistant Professor with expertise in health psychology and maternal mental health. Dr. Kwitowski treats psychotherapy patients in the peripartum period and serves as lead psychologist for an integrated behavioral health service that provides behavioral health support for women and families hospitalized in the immediate postpartum period. The primary focus of the program is perinatal mental health concerns, substance use, maternal-fetal complications, and traumatic obstetric outcomes.
Dr. Rayna D. Markin will review types and rates of pregnancy loss and common psychological consequences for bereaved parents, including anxiety, depression, complicated grief, and post-traumatic stress. Moving beyond a symptomatic focus, she will focus on the deeper level psychological effects of pregnancy loss, including unresolved trauma and loss and damage to healthy self-esteem and identity. Dr. Markin will also discuss the therapy relationship as a vehicle to help patients process and grow from trauma and loss and restore healthy self-esteem after experiencing pregnancy loss. Special implications for BIPOC and LGBTQ+ clients will be discussed.
1.5 CE Credits, Instructional Level: Intermediate
1.5 Contact Hours (New York Board of Psychology)
Learning Objectives:
Disclosures: Dr. Markin has no conflicts of interest to disclose.
Rayna D. Markin, PhD, received her doctorate in Counseling Psychology from the University of Maryland, College Park and is currently an Associate Professor in counseling at Villanova University and a licensed psychologist with a private practice. She is founder of the Therapy Center for Pregnancy Loss, LLC. She is the author of the new book Psychotherapy for Pregnancy Loss: Applying Relationship Science to Clinical Practice, and co-author of the book Attachment in Group Psychotherapy
From 1973 until 2022, people who no longer desired to be pregnant in the United States were able to access safe and legal procedures to terminate pregnancies. Pregnancy termination is complex not only for the society and culture we are steeped in, but also for the individuals and families that experience them. Dr. Julie Bindeman will review psychosocial aspects of abortion for varied reasons (e.g., fetal anomalies, mother’s health, sexual assault, personal choice, etc.). Dr. Bindeman will also review clinical and practice management issues, interjurisdictional challenges, and documentation recommendations. Case examples will illustrate best practices in care at this time.
1 CE Credit, Instructional Level: Intermediate
1 Contact Hour (New York Board of Psychology)
Learning Objectives:
Disclosures: Dr. Bindeman is the current Chair of the Mental Health Professional Group of the American Society of Reproductive Medicine.

Julie Bindeman, PsyD, graduated from George Washington University and is the co-owner of Integrative Therapy of Greater Washington in Rockville, MD. Her specialty is in the field of Reproductive Psychology. She is an approved consultant in EMDR through EMDRIA as well as a facilitator for basic training with The Touchstone Institute. She has served on several committees within the Mental Health Professional Group of the American Society for Reproductive Medicine and was elected in 2021 to its Executive Committee.
With 1 in 6 individuals experiencing infertility challenges with their family building, infertility is a major life event that introduces the stress and burden of uncertainty in addition to the demands of treatment. Research has demonstrated that the infertility experience contributes to similar levels of depression and anxiety as navigating the experience of cancer. Dr. Andrea Braverman will discuss the mental health impact of infertility challenges and review evidence-based interventions for various populations.
2 CE Credits, Instructional Level: Intermediate
2 Contact Hours (New York Board of Psychology)
Learning Objectives:
Disclosures: Dr. Braverman has no conflicts of interest to disclose.

Andrea Braverman, PhD, is a Clinical Professor with a joint appointment in the Department of Obstetrics and Gynecology and Psychiatry and Behavioral Medicine at Thomas Jefferson University. Dr. Braverman is the Associate Director for the Educational Core for OB/Gyn and the Director of the College Learning Environment at Sidney Kimmel Medical College. She is a health psychologist with a specialty in medical health management, infertility counseling, and third-party reproduction issues. She received her MA, MS, and PhD from the University of Pennsylvania.
Dr. Wiyatta Fahnbulleh will focus on the critical role of cultural humility in delivering effective and inclusive care for patients navigating obstetrics and reproductive medicine. She will examine how cultural dynamics, systemic barriers, and communication styles influence patient experiences and clinical outcomes. Using case studies and research-informed strategies, she will explore actionable approaches to enhance cultural sensitivity and patient-centered care. Dr. Fahnbulleh will aim to equip professionals with the tools needed to improve patient care and collaboration within interdisciplinary reproductive health settings.
1 CE Credit, Instructional Level: Intermediate
1 Contact Hour (New York Board of Psychology)
Learning Objectives:
Disclosures: Dr. Fahnbulleh has no conflicts of interest to disclose.

Wiyatta Fahnbulleh, PsyD, is a licensed clinical, forensic, and reproductive psychologist. She integrates clinical practice with speaking, writing, content creation, and consultations. Specializing in helping professional women navigate career challenges, life transitions, and fertility issues, she offers fertility counseling, intended parent consultations, and third-party evaluations. She chairs the ASRM Mental Health Professional Group’s Diversity, Inclusion, and Anti-Racism Committee. Dr. Wiyatta earned her PsyD in Clinical Forensic Psychology from The Chicago School of Professional Psychology, Los Angeles.
Dr. Tonya Wood will review patient-identified challenges with current obstetrics/gynecology and reproductive medicine practices for procedural preparation. During this skills-focused workshop, brief interventions will be reviewed for persons preparing for labor and delivery, c-sections, delivery after prior pregnancy complications and loss, IVF, and other reproductive medicine procedures. In addition, Dr. Wood will provide strategies to identify persons at risk for emotional distress before and during obstetrical and reproductive medicine procedures. She will also highlight communication strategies with family members, OB, and reproductive medicine teams to improve patients’ experience before, during, and following procedures.
1 CE Credit, Instructional Level: Intermediate
1 Contact Hour (New York Board of Psychology)
Learning Objectives:
Disclosures: No conflicts of interest to disclose.

Tonya Wood earned her PhD in Clinical Psychology at the University of Virginia and currently serves as the Director of Clinical Training in the PsyD program at Pepperdine University. She has a private practice specializing in infertility and reproductive health. Dr. Wood has worked in various academic and public sector settings, with an emphasis on providing quality and effective services to marginalized populations. She was 2020 President of the California Psychological Association. In 2023 she was awarded a Presidential Citation from the American Psychological Association for her work in reducing disparities in access to care and infertility.
All too many persons receiving care in obstetrical, gynecological, and reproductive medicine settings have experienced trauma in their past, more recently than and/or concurrently with treatment. Dr. Helen L. Coons will highlight essential components of trauma-informed care when individuals are facing obstetrical, gynecological, or infertility procedures. Integrated and community-based psychologists can effectively offer trauma-informed care and collaborate with clinical providers to improve patient experiences, outcomes, and well-being. Dr. Coons will provide case discussions that focus on clinical approaches for patients from diverse communities with histories of child sexual abuse, sexual assault, interpersonal violence, or medical trauma who are receiving care in OBGYN and reproductive medicine.
1.5 CE Credits, Instructional Level: Intermediate
1.5 Contact Hours (New York Board of Psychology)
Learning Objectives:
Disclosures: Dr. Helen L. Coons has no conflicts of interest to disclose. Generative AI was not used in the production or content of this curriculum.

Helen L. Coons, PhD, ABPP, is the President and Clinical Director of Women’s Mental Health Associates and Health Psychology Solutions, Denver, Colorado. She is a board-certified clinical health psychologist known for her clinical work and integrated services in women’s health settings. Dr. Coons has worked with women and couples facing PCOS, infertility, recurrent pregnancy loss, perinatal mental health conditions, breast and gyn cancers, menopause, and sexual health challenges for over three decades.
Polycystic ovary syndrome (PCOS) is a common, yet under-recognized, endocrine condition, affecting 11-13% of females globally. People with PCOS have a three- and four-fold risk for developing depression, anxiety, and eating disorders, yet psychologists receive limited education and training to address the biopsychosocial and cultural determinants of PCOS-related mental health concerns. Dr. Phimphasone-Brady will address the need for improved clinician education in the comprehensive management of PCOS, discuss the current international guidelines and issues relevant to improving mental health and well-being in PCOS, and review specific evidence-based interventions and strategies for addressing the overwhelming mental health needs in PCOS.
1.5 CE Credits, Instructional Level: Intermediate
1.5 Contact Hours (New York Board of Psychology)
Learning Objectives:
Disclosures: Dr. Phimphasone-Brady has no conflicts of interest to disclose.

Phoutdavone Phimphasone-Brady, PhD, is an Assistant Professor in the Department of Psychiatry at the University of Colorado Anschutz Medical Campus. As a licensed clinical health psychologist and implementation scientist, her expertise is on the prevention and management of mental and behavioral health concerns in female-specific medical conditions (e.g., polycystic ovary syndrome) and the implementation and dissemination of innovative interventions and programs with multi-level partners and collaborators to promote equitable health care access for comprehensive and whole person care.
Dr. Christina Metcalf and Dr. Nanette Santoro will cover essential aspects of menopause, focusing on its stages, symptoms, and the best practices for both short- and long-term management strategies. Attendees will gain a comprehensive understanding of perimenopause and the menopause transition and their impacts on health and mental health, with a special focus on psychosocial interventions and shared decision-making. Drs. Metcalf and Santoro will prepare clinicians to implement effective strategies to help their patients manage menopausal symptoms. Participants will gain practical knowledge to help support women during this important phase of life.
2 CE Credits, Instructional Level: Intermediate
2 Contact Hours (New York Board of Psychology)
Learning Objectives:
Disclosures for Dr. Metcalf: No conflicts of interest to disclose. Generative AI was not used in the development or content of this presentation.
Disclosures for Dr. Santoro:
Generative AI was not used in the development or content of this presentation.
Active Non-Disclosures; Astellas Pharma, Member of Scientific Advisory Board & Medical Affairs Steering Committee; Ansh Labs, Scientific Consultant; Novo Nordisk, Consulting Services Agreement; Bayer Consumer Care AG, Consulting Services Agreement; and Perrigo/Laboratoire HRA PHARMA, Consulting Services Agreement

Christina Metcalf, PhD, is a clinical psychologist and Assistant Professor at the Colorado Center for Women’s Behavioral Health and Wellness, Department of Psychiatry within the University of Colorado Anschutz Medical Campus. She centers her research and clinical work on understanding and ameliorating mental health concerns during the menopause transition. Dr. Metcalf’s research has contributed to increased awareness of the individual risk factors that may amplify menopause-related cognitive concerns and depression symptoms with the goal of improving brain health during this transition.

Nanette Santoro, MD, is the E Stewart Taylor Chair of Obstetrics & Gynecology at the University of Colorado School of Medicine, where she has served for 14 years. She has been continuously funded by the NIH since 1989 for research in female reproduction. Her work has covered the processes of the pubertal and menopausal transition, as well as clinical trials in reproduction and menopause. She has headed studies of women with premature and age-appropriate menopause such as the Women’s Health Initiative and the Kronos Early Estrogen Prevention Study (KEEPS), and the Study of Women’s Health Across the Nation (SWAN). Dr. Santoro has held numerous leadership positions in local and national organizations. She is immediate Past President of the Society for Reproductive Investigation. In 2018, Dr. Santoro was elected to the National Academy of Medicine.
Women have typically been overlooked when it comes to issues with their sleep. Unfortunately, many women have also been told that poor sleep comes with the territory. Dr. Shelby Harris will focus on common sleep issues women face and will discuss evidenced-based treatment options for these issues and disorders as well as when to refer to a sleep center. She will also provide an introduction to Cognitive Behavior Therapy for Insomnia because insomnia is the most common sleep issue women face at various stages in life.
2 CE Credits, Instructional Level: Intermediate
2 Contact Hours (New York Board of Psychology)
Learning Objectives:
Disclosures: Dr. Harris has no conflicts of interest to disclose.

Shelby Harris, PsyD, DBSM, is a clinical psychologist in private practice in NY. She is board certified in Behavioral Sleep Medicine (BSM) and treats a wide variety of sleep, anxiety, and depression issues using evidence-based, non-medication treatments. Her book The Women’s Guide to Overcoming Insomnia was published in 2019 by W.W. Norton Books. Dr. Harris holds an academic appointment as Clinical Associate Professor at the Albert Einstein College of Medicine in Neurology and Psychiatry.
Health psychologists need a deep understanding of women’s sexual health across the lifespan to address its complex biological, psychological, relational, and sociocultural dimensions. Dr. Stephanie Buehler will discuss an inclusive framework that explores cultural and systemic factors that shape sexual health, including the experiences of LGBTQ+ women and those from diverse racial and ethnic backgrounds. She will also discuss practical, evidence-based strategies to integrate culturally responsive and affirmative approaches into practice. Through case examples and actionable insights, Dr. Buehler will empower psychologists to assess, intervene, and advocate for women’s sexual well-being.
2 CE Credits, Instructional Level: Intermediate
2 Contact Hours (New York Board of Psychology)
Learning Objectives:
Disclosures: Dr. Buehler has no conflicts of interest to disclose.

Stephanie Buehler, MPW, PsyD, CST-S, IF, is a licensed psychologist and sex therapist and a Fellow of the International Society for the Study of Women’s Sexual Health. She is the author of What Every Mental Health Provider Needs to Know about Sex (3rd ed.) and founder of The Buehler Institute, which offers continuing education in sex and relationship therapy.
Chronic health conditions, which become more prevalent with age, affect more than 38% of women in the United States. Women’s distinct physiology and the impact of adverse life experiences contribute to the higher prevalence and severity of these conditions. Drs. Kathleen Brown and Jennifer Kelly will explore the reasons behind these patterns and offer practical strategies for practitioners to alleviate suffering and enhance wellness.
2 CE Credits, Instructional Level: Intermediate
2 Contact Hours (New York Board of Psychology)
Learning Objectives:
Disclosures: Dr. Brown and Dr. Kelly have no conflicts of interest to disclose.

Kathleen S. Brown, PhD, is a licensed psychologist specializing in health and rehabilitation psychology. She is currently involved in consulting, teaching, and supervision in her independent consulting practice in Fort Myers, FL. Dr. Brown served on the APA/APASI Board of Directors as Recording Secretary (2022-2024); is a member-at-large on the Board of the Foundation of Rehabilitation Psychology; was President of the Division of Rehabilitation Psychology (22) and the Hawai’i Psychological Association; and is a fellow of the American Psychological Association (APA; Divisions 22, 31, 38, 55).

Jennifer F. Kelly, PhD, ABPP, is a licensed psychologist and is Board Certified in Clinical Health Psychology. She served as the 2021 President of the American Psychological Association. Her presidential initiatives focused on Psychology’s Role in Achieving Health and Racial Equity. She is the director of the Atlanta Center for Behavioral Medicine in Atlanta, Georgia. Dr. Kelly addresses a variety of mental health concerns in her practice, with expertise in treating disorders that involve the relationship between physical and emotional conditions
One in eight women will be diagnosed with breast cancer, with profound impact on their life beyond physical health, including mental health, body image, career, and relationships. Dr. Kathleen Ashton will focus on the latest research in psychosocial oncology and best practices in treatment of patients affected by breast cancer. The psychological needs of diverse patients will be discussed, including those with hereditary risk, in active treatment, in survivorship, or with metastatic breast cancer, as well as patients from BIPOC and LGBTQ+ populations. Dr. Ashton will also include case discussions and interactive clinical application exercises.
2 CE Credits, Instructional Level: Intermediate
2 Contact Hours (New York Board of Psychology)
Learning Objectives:
Disclosures: Dr. Ashton has no conflicts of interest to disclose.

Kathleen Ashton, PhD, ABPP, FACHP, is a Board Certified Clinical Health Psychologist at the Cleveland Clinic since 2004, where she is the Director of Behavioral Health for the Breast Center and an Associate Professor of Surgery in the Lerner College of Medicine. Her clinical and research interests include psychosocial aspects of breast cancer and hereditary risk of breast cancer. She is a fellow of the American Psychological Association and Past President of APA Division 31.
As our aging population continues to grow, women’s health and aging are expected to become areas of increasing clinical focus for psychologists. Older adult women are projected to be a large portion of the aging population and with advanced age comes increased likelihood of multiple medical conditions and associated functional changes. Additionally, personal beliefs about aging can influence one’s engagement in health behavior, life satisfaction, and mental health wellbeing. Dr. Nicole Reynolds will explore how aging impacts older adult women and discuss strategies for how to promote aging well through a biopsychosocial lens including reframing aging, addressing functional limitations, planning for end-of-life, and risk mitigation strategies.
2 CE Credits, Instructional Level: Intermediate
2 Contact Hours (New York Board of Psychology)
Learning Objectives:
Disclosures: Dr. Reynolds has no conflicts of interest to disclose.

Nicole Reynolds, PsyD, ABPP, is a licensed clinical psychologist with a background in health psychology and integrated care. She is board certified in geropsychology. She has worked with older adults across medical settings including primary care, oncology, palliative care, solid organ transplant, and private practice. She is currently working as an Assistant Professor at the University of Colorado School of Medicine (CUSOM) in the transplant surgery department and in outpatient faculty practice.
Dr. Lindsay Lebin will explore sex and gender differences in psychopharmacology, focusing on the unique needs of women across the lifespan. After reviewing the reproductive life cycle in women, Dr. Lebin will examine gender-specific considerations related to pharmacokinetics, pharmacodynamics, and social factors at different stages of reproductive transition. By highlighting key research findings and clinical implications, Dr. Lebin will review gender-informed approaches to psychopharmacology.
1 CE Credit, Instructional Level: Intermediate
1 Contact Hour (New York Board of Psychology)
Learning Objectives:
Disclosures: Dr. Lebin has no conflicts of interest to disclose.

Dr. Lindsay Lebin received her MD from the University of Colorado. She completed psychiatry residency at the University of Washington and consultation-liaison psychiatry fellowship at University of California San Francisco. She is currently an Assistant Professor in the Department of Psychiatry at the University of Colorado School of Medicine. Her clinical interests include integrated care, psychosocial oncology, and reproductive psychiatry. She serves as the Director of Psychiatry Trainees in Women’s Behavioral Health and Wellness and engages in scholarly work in medical education.
Dr. Sarah Burgamy will focus on the intersection of health care and sex, sexual orientation, and gender identity. Specifically, she will explore this intersectionality in light of how clinical approaches to health and wellness may differ in gender and sexual orientation diverse people. Mental health providers will learn a functional way to approach patients inclusive of cisgender women, transgender and gender diverse (TGD) assigned female at birth (AFAB) individuals with respect to many aspects of health care. Finally, Dr. Burgamy will explore considerations of sexual orientation and diverse relational orientations as they apply to speaking to patients about health and wellness (e.g., family planning, health of sex-specific organs, care for medical conditions such as breast/chest and gynecological cancers in traditional women’s health settings, and culturally competent aspects of making health care referrals). She will highlight case examples of effective clinical and collaborative strategies for mental health providers to improve the health and wellbeing of cisgender women as well as people who are transgender and gender diverse AFAB people.
1.5 CE Credits, Instructional Level: Intermediate
1.5 Contact Hours (New York Board of Psychology)
Learning Objectives:
Disclosures: Dr. Burgamy has no conflicts of interest to disclose.

Sarah E. Burgamy, PsyD, is a clinical psychologist with nearly 20 years of clinical expertise working with children, adolescents, and adults. The primary foci of her clinical work, professional trainings, and speaking engagements are gender and sexual orientation diversity across the lifespan. Dr. Burgamy has served as a past chair of the APA Committee on Sexual Orientation and Gender Diversity and past chair of the Leadership Institute for Women in Psychology Advisory Committee.
Dr. Helen L. Coons will review ten clinical strategies to promote health and well-being in women across the lifespan. While profoundly resilient, women all too often cope with undertreated complex and interacting physical conditions, anxiety, insomnia, relentless fatigue, depression, trauma, work-place discrimination, and caregiver burden among other determinants of poor health and mental health. These challenges are even more common in persons from minoritized and marginalized communities. Dr. Coons will discuss robust treatment and prevention interventions aimed at supporting women’s physical, psychological, relational, sexual, and economic health.
1 CE Credit, Instructional Level: Intermediate
1 Contact Hour (New York Board of Psychology)
Learning Objectives:
Disclosures: Dr. Helen L. Coons has no conflicts of interest to disclose. Generative AI was not used in the production or content of this curriculum.

Helen L. Coons, PhD, ABPP, is the President and Clinical Director of Women’s Mental Health Associates and Health Psychology Solutions, Denver, Colorado. She is a board-certified clinical health psychologist known for her clinical work and integrated services in women’s health settings. Dr. Coons has worked with women and couples facing PCOS, infertility, recurrent pregnancy loss, perinatal mental health conditions, breast and gyn cancers, menopause, and sexual health challenges for over three decades.
Licensing boards have specific requirements for the number of CEs and types of CE needed for license renewal. Each licensing board is the primary source of information on these requirements. If you have license renewal questions, please contact your licensing board. We have board websites listed online.
The National Register of Health Service Psychologists is approved by the American Psychological Association to sponsor continuing education for psychologists. The National Register maintains responsibility for this program and its content.
The National Register of Health Service Psychologists is recognized by the New York State Education Department’s State Board for Psychology as an approved provider of continuing education for licensed psychologists #PSY-0010.
